The assurance of lasting immunity for people who have recovered from COVID-19 changes the game in the fight against the pandemic.
This immune group (57 million people worldwide) is increasing almost as fast as the number of people infected by the coronavirus (80 million).
COVID-19 cases in general last for between two and three weeks and 98% of infected people recover without too many problems. They develop immunity which prevents them from catching the disease again. So the patterns of infection and recovery thus match each other closely with a lag of just a few weeks.
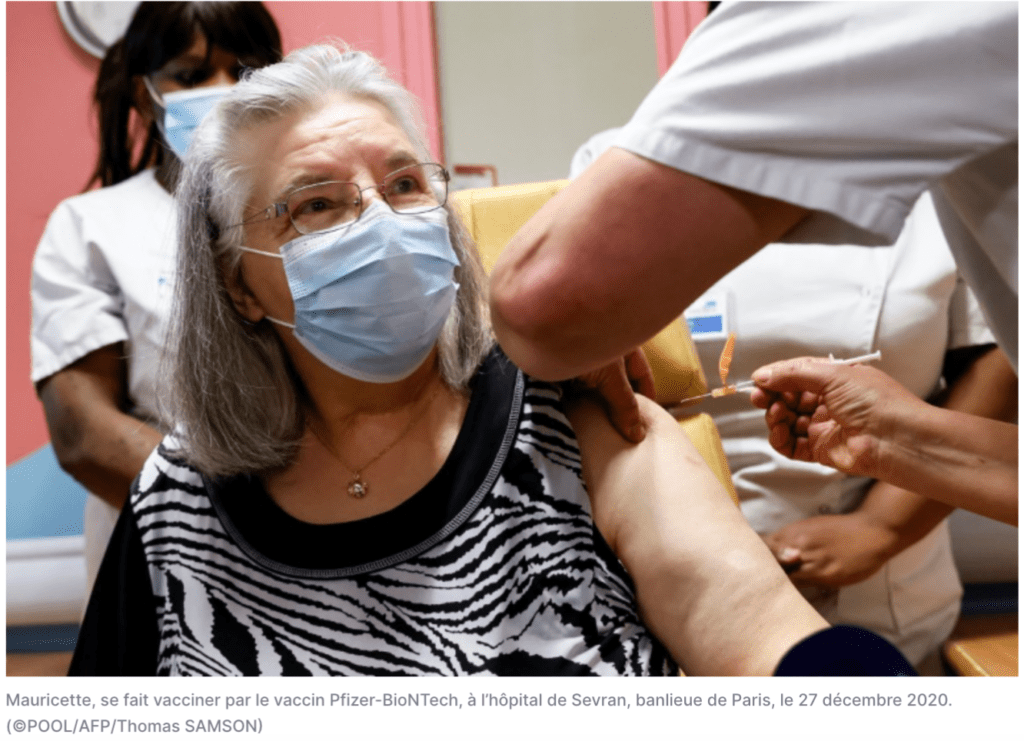
As countries prepare to massively vaccinate their populations in the face of numerous uncertainties, ignoring the immunological status of those who have recovered would be negligent in a context where scarcity must be managed.
A race against time
On a global level, these vaccination campaigns are a race against time where lack of resources will impose cruel dilemmas as to which lives are to be saved first. Rapid action is needed through deliberate choices to take account of the constraints in terms of health, money and logistics which have never before been experienced on such a scale.
The situation recalls the most difficult moments of the crisis last spring when doctors, faced with an unprecedented surge of hospital admissions, had to decide which people they would try to save and which they had to leave to die.
Given the colossal scale of the vaccination campaigns to be carried out, the precious vaccines which have just been developed could run out at any time and in any place, especially in the poor countries of Africa and Asia. The health authorities will have to make tough, but rational choices.
In France, the HAS health authority has issued an ambiguous recommendation according to which "there is no need to systematically vaccinate people who have already been contaminated by coronavirus, but there is no reason why this can’t be done." This is a classic example of bureaucratic language which avoids taking a risk and accepting responsibility.
But when the HAS states that the "scientific observation" is that "to date the information does not allow us to know if there is a benefit from vaccinating people who have already been infected by SARS-CoV-2," it acknowledges that, in the current state of knowledge, it would be pointless to vaccinate those who have been sick and are now immune.
Pointless is the key word. If a rich country like France can afford to, for reasons which are outside the health domain, undertake obviously pointless initiatives, this is not the case in many poor countries in Africa and Asia which are still asking how they can find the financial and logistical means to vaccinate even a small part of their populations.
WHO Role
It is urgent for countries and especially for the World Health Organization to draw clear conclusions and make operating recommendations on the basis of current scientific knowledge. Yet there is nothing that is absolutely free of risk, as is true for the vaccines which several countries have authorised but for which there is not yet a 100% guarantee of effectiveness or absence of side-effects.
This is also true for the immunity naturally acquired by those who have had COVID-19 and have recovered. There is no question of putting this natural immunity and the immunity acquired by vaccination into competition. It’s simply a matter of accepting facts and using them to the best advantage for public health.
Naturally acquired immunity after infection with COVID-19 is indeed real and lasts at least as long as the immunity generated by the new vaccines, based on rigorous scientific observation.
While the newly approved vaccines (Pfizer/BioNTech, Moderna, AstraZeneca) have effectiveness rates reaching 95% among those given experimental vaccines in the last three to six months, practically 100% of those who have been ill with COVID-19 have not become sick again over the last nine to twelve months. In fact, of the 57 million people globally who have been ill with symptoms to date, only a few dozen have become ill again. These cases are the exceptions which prove the rule of real and lasting immunity.
The lesson is clear: in poor or heavily populated countries where vaccines won’t be available for the whole population in 2021 or 2022 and where priorities must be defined to safeguard the lives of millions of people, those who have been ill with COVID-19 and shown symptoms as well as a positive polymerase chain reaction (PCR) test should not be among the first to benefit from the coming vaccination campaigns. Priority must be given to more vulnerable people who have not yet met with the coronavirus.
To manage the health crisis better, authorities should define a special status for those who have been ill with COVID-19 and have been registered as such in the past. This status can be consolidated and extended to those who have been contaminated even without experiencing any symptoms, by a serological test showing the presence of antibodies showing humoral immunity against the pathogen, given that everyone who has had the sickness will also have developed cellular immunity represented by the T lymphocytes, or killer cells.
In practical terms, the status of those who have been ill and are now recovered is close to that of vaccinated people, who will also have produced antibodies, notably the IgG antibodies which are the most effective and long-lasting.
Such a special status for the ones who have recovered would avoid putting everyone to be vaccinated in the same basket and allow a better allocation of these precious vaccines.
Sam Rainsy