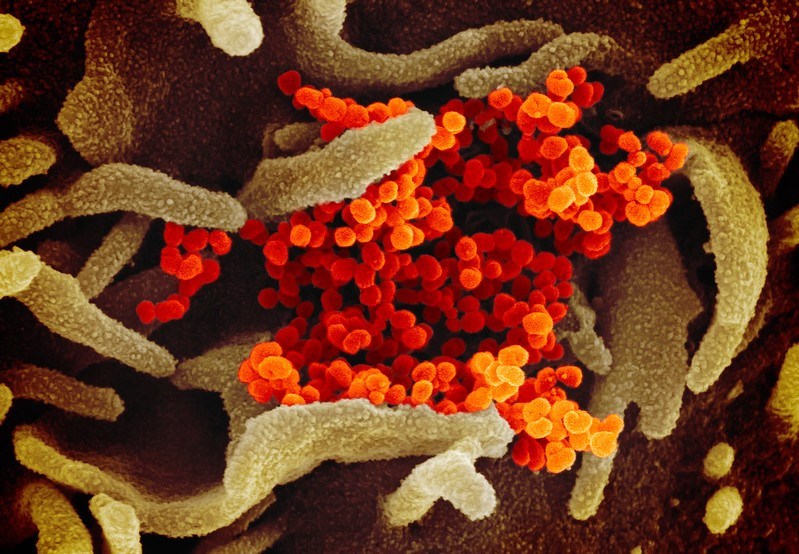
The European Centre for Disease Prevention and Control (ECDC) published on Monday a technical report on the introduction and prioritisation of COVID-19 vaccination in the EU/EEA and the UK.
The Centre writes that the aim of the report is to support but not to define EU policy on COVID-19 vaccination. Foreseeing a possible lack of coordination in the EU, it adds that an “EU-wide approach will be crucial in the interest of solidarity, equity, accessibility and ultimately halting the threat to citizens’ health posed by COVID-19”.
Currently, there is a lack of certainty and knowledge about the characteristics of COVID-19 vaccines that could become available in the EU/EEA and the UK, as well as remaining gaps in the scientific knowledge of the virus and the disease. According to the report, there is no approved COVID-19 vaccine for use in the EU/EEA and the UK.
However, several candidate vaccines are undergoing human trials, with nine vaccine candidates having entered phase II/III or phase III clinical trials globally. It is currently unknown when potential COVID-19 vaccines will be authorized for use in the EU/EEA and the UK.
The European Medicines Agency (EMA) has stated that in a best-case scenario the agency would receive clinical data on the most advanced vaccines towards the end of 2020. It is expected that once COVID-19 vaccines are authorised and available the doses will initially be limited, so there will be a need to prioritise those target groups that should be vaccinated first.
Given this anticipated initial shortage, countries will need to identify priority groups for vaccination to be optimally further characterised into tiers.
“The identification of priority groups for vaccination will depend on several factors, which are outlined in the technical report. Most importantly, vaccine allocation needs to be promptly optimised and vaccine availability to those most in need should be ensured,” said Andrea Ammon, Director of ECDC (26 October).
The report lists the following non-mutually exclusive approaches for vaccine deployment, taking into account different levels of vaccine supply and stages of the pandemic:
* focusing on selected groups (e.g. individuals at risk of severe COVID-19, essential workers, vulnerable groups);
* vaccinating according to age strata (e.g. all individuals above a certain age);
* targeting groups with an increased risk of exposure and onward transmission of SARS-CoV-2 (e.g. exposure in professional settings, younger adults);
* prioritising geographical regions with high incidence of COVID-19;
* deploying the vaccine to control active outbreaks;
* performing adaptive approaches to be modulated according to circumstances;
* conducting a universal vaccination strategy.
As regards protective immunity following natural COVID-19 infection, the report states that scientific evidence is currently limited. Since the immunological correlate for protection is not yet fully established, it is also difficult to estimate what an observed vaccine-induced immune response means.
Moreover, there is currently limited information on the duration of immunity following natural infection. A few reported cases of reinfection have been observed. It is considered possible that a previous infection confers protection for around six months, although this may also vary across age groups and between severe, mild and asymptomatic cases.
The Brussels Times