World Cancer Day (4 February) falls just days after the appointment of a new Belgian Government this year. One key organisation fighting against cancer, Kom op tegen Kanker, has reacted positively to some proposed policies, but argues there is still a long road ahead.
Over the past decade, the share of deaths linked to cancer in Belgium has decreased significantly, the 2025 Cancer Report published by the OECD and European Commission showed. Still, over 26,000 people in the country die of some form of cancer every year, making it the leading cause of death.
The number of new cancer diagnoses every year (cancer incidence) is higher than the EU average. "Around 76,220 new cases of cancer were counted in the country [in 2022]," Kom op tegen Kanker's Sven Haenen told The Brussels Times. By 2030, this figure is expected to rise to 83,590 every year.
Weighing costs
Cancer prevalence – the number of living people who have ever been diagnosed with cancer – has been growing by around a quarter between 2010 and 2020 in EU countries. For this reason, governments are increasingly investing in improving cancer care, from prevention and diagnosis to support for patients and post-cancer care. This was reflected in the agreement of the next Federal Government.
In the wake of the government formation, Kom op tegen Kanker analysed how the various proposals will impact cancer care and patients. "Our main disappointment is that the government will not be tackling high medicine prices," said Haenen.
The organisation has long opposed the high prices of (new) cancer drugs. It argues that firms are trying to maximise profits by pushing the limit of how much countries are willing or able to pay. Nivolumab, for example, is an immunotherapy used to treat lung cancer and melanoma (a type of skin cancer), among others. It costs Belgian health insurance companies about €38,000 per patient per year.
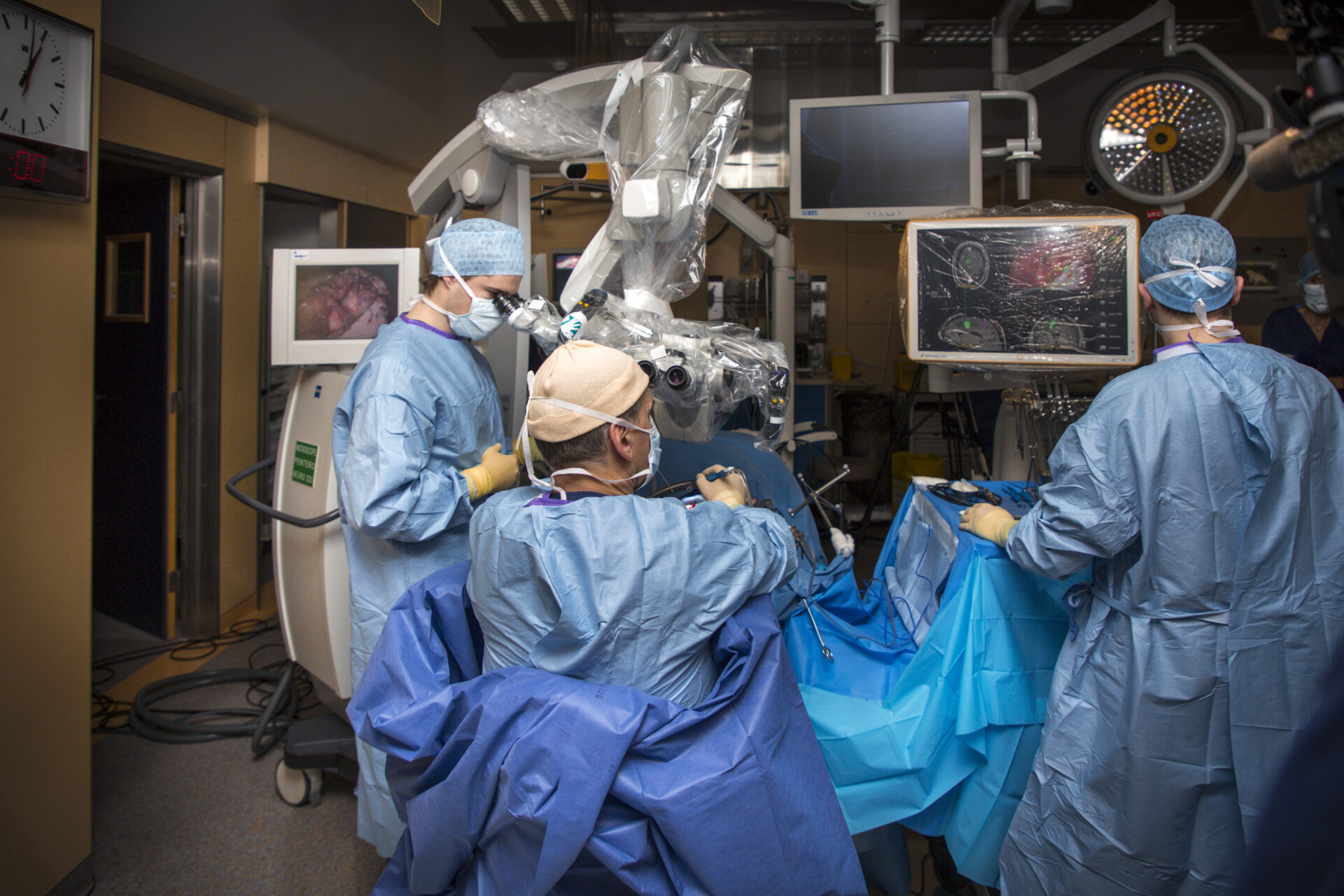
Credit: Belga / Hatim Kaghat
In poorer countries, this leads to unequal access to treatment. In Belgium, this puts pressure on the country's healthcare budget: spending on such medication increased by 15% annually between 2014 and 2019. "Such growth is unsustainable, and therefore a threat to accessible healthcare," the organisation noted.
The organisation also laments that the tax deduction on donations will drop from 45% to 30%. As a result, donations to charities relying on income from donations, such as Kom op tegen Kanker, are expected to decrease.
"Finally, more work must be done around the reintegration of cancer patients into everyday life. We are calling for improved cooperation between all stakeholders. We also call on the government to stop seeing people who are diagnosed with cancer as victims," Haenen concluded.
Positive notes
However, Belgium is also a pioneer on many fronts. It is one of the few EU countries to use self-sampling tests as part of screening efforts. It has also implemented specialised psycho-oncology services, incorporating mental health care into standard cancer treatment, the 2025 Cancer Report highlighted.
Regarding policies put forward by the new 'Arizona' government, Kom op tegen Kanker welcomed several actions focusing on smoking (the main preventable cause of cancer and other diseases), vaping and alcohol consumption.
The new Federal Government will look into banning smoking rooms in publicly accessible institutions, making tools that help people quit smoking more accessible through health insurance. It is also considering extending the smoking ban to terraces, which Kom op tegen Kanker says will help smokers quit more easily.
Related News
- Alcohol-related deaths surged in past decade
- Tumours or falls: What are Belgium's most common causes of death?
- Less radiotherapy needed for people with operable breast cancer
Regarding alcohol consumption, the current government line "alcohol abuse damages health" will be replaced by "alcohol damages health" to indicate there is no such thing as a healthy level of alcohol consumption.
Finally, Stichting tegen Kanker, another pivotal organisation fighting against cancer, welcomed that the coalition agreement includes the objective of a new Cancer Plan (the previous one dates back to 2008). It will promote early screening and expand the funding and capacity of care facilities.